Treatment Options for Metastatic Brain Tumors
1. Introduction: Why This Guide Matters
Receiving a diagnosis of a metastatic brain tumor can be a deeply unsettling experience for both patients and their families. But this diagnosis does not always mean there are no options. Today, thanks to advanced imaging, molecular profiling, and targeted treatments, significant progress has been made in the management of these tumors.
This guide was created to help you understand the available treatment options and to answer the most common questions we hear from newly diagnosed patients. Our goal is to present complex medical information in a clear and accessible way, helping you feel empowered to make informed decisions.
2. How Is a Treatment Plan of Metastatic Brain Tumors Created?
Treatment plans for metastatic brain tumors are highly personalized. Every patient has a different cancer type, pattern of spread, and overall health status. There is no one-size-fits-all solution.
Several factors are considered when planning treatment:
- Number, location, and size of brain metastases
- Type of primary cancer and whether it has spread to other organs
- Patient’s age, general health, and coexisting conditions
- Previous treatments and how well they worked
This process is guided by a multidisciplinary team. In comprehensive cancer centers such as Anadolu Medical Center in Turkey, each patient’s case is reviewed in a tumor board by specialists from neurology, neurosurgery, medical oncology, and radiation oncology. Together, they create a tailored treatment strategy based on current evidence and the individual needs of the patient.
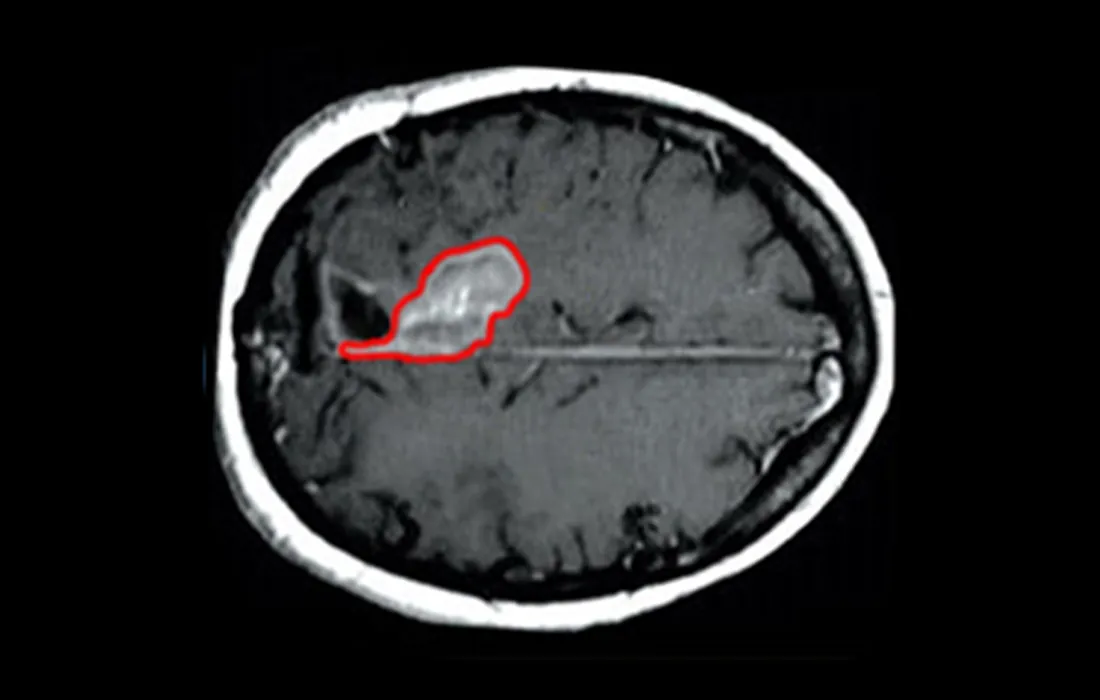
3. Surgical Intervention
When there are a limited number of brain metastases in accessible locations, surgery can be a very effective option. It is often used to quickly reduce pressure in the brain caused by a large tumor or swelling.
Key benefits of surgery include:
- Immediate removal of tumor tissue
- Rapid relief of neurological symptoms
- Pathological confirmation of diagnosis
- Better conditions for follow-up treatments such as radiosurgery
Surgery is not suitable for every patient. The location of the tumor, its size, and the patient’s general health must all be carefully evaluated.
4. Stereotactic Radiosurgery (Gamma Knife, CyberKnife)
This non-invasive treatment delivers high-dose radiation to a very precise area, making it ideal for patients with 1–4 small metastases who are not candidates for surgery.
- No incisions; treatment is delivered externally
- Targets the tumor while sparing healthy brain tissue
- Usually completed in a single session
- Fast recovery, often without the need for hospitalization
Radiosurgery is increasingly becoming a first-line treatment for many patients due to its safety and effectiveness.
5. Whole Brain Radiation Therapy (WBRT)
If there are multiple or widespread metastases in the brain, whole brain radiation therapy may be recommended.
- Helps treat both visible tumors and microscopic disease
- Typically delivered over 10–15 sessions
- May cause cognitive side effects (memory loss, difficulty concentrating) over time
Newer techniques aim to reduce these side effects, but WBRT is generally reserved for specific situations where other options are not viable.
6. Systemic Therapies: Targeting the Cancer Throughout the Body
Since brain metastases are part of a systemic disease, treatment must also address cancer throughout the body.
a. Chemotherapy
Chemotherapy can be effective for certain cancers, such as small cell lung cancer. However, many drugs cannot cross the blood-brain barrier effectively, limiting their impact on brain metastases.
b. Targeted Therapies
These drugs are designed to attack specific genetic mutations in cancer cells.
- EGFR, ALK, ROS1 mutations (often in lung cancer) respond well to certain oral targeted therapies
- These medications can reach brain metastases and control disease for extended periods in some patients
c. Immunotherapy
This approach activates the immune system to fight cancer.
- Shown to be effective in melanoma and certain lung cancers
- May also impact brain metastases in selected patients
- Often used in combination with other treatments
Genetic testing is often needed to determine if these therapies are appropriate.
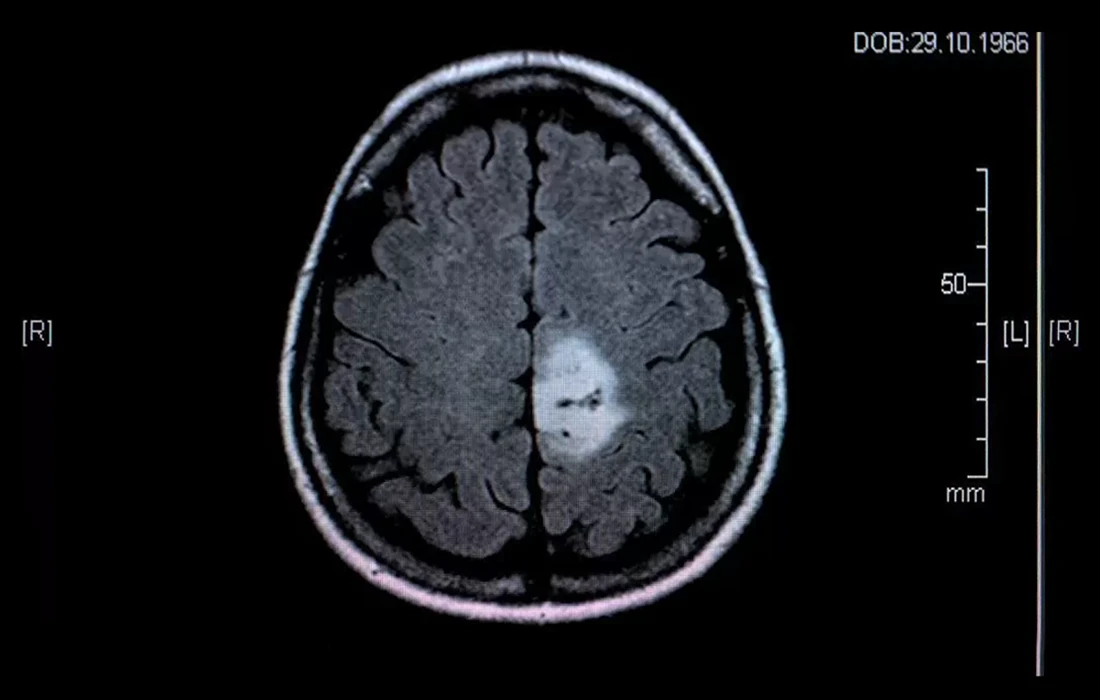
7. Monitoring and Follow-Up
Once treatment begins, close monitoring is essential.
- Follow-up MRIs help assess response to treatment
- Tumor size and appearance are evaluated over time
- Adjustments to the treatment plan may be made as needed
Some patients require only one type of treatment, while others benefit from a combination over time. Flexibility and individualized care are key.
8. Frequently Asked Questions
Can the tumor return after treatment?
Yes, recurrence is possible. That’s why regular imaging and follow-up are critical.
Will I be able to return to daily life after surgery or radiosurgery?
In most cases, yes. Many patients experience a noticeable improvement in symptoms and quality of life after treatment.
Are the treatments painful?
No. Stereotactic radiosurgery is painless. Surgery may cause temporary discomfort, but pain is usually well controlled.
Will I lose functions like vision, speech, or balance?
This depends on the tumor’s location. However, with modern surgical and radiation techniques, such complications are much less common than in the past.
9. Conclusion: There Is Reason for Hope
Metastatic brain tumors no longer represent a hopeless situation. Thanks to scientific advances, we now have more precise diagnostic tools, more targeted treatment options, and improved quality-of-life outcomes.
Every case is unique. But with the right team, timely intervention, and a patient-centered approach, many people can continue their lives with strength and stability after a diagnosis.
If you or a loved one is facing this diagnosis, know that you are not alone. The most important first step is to get informed and seek care from a trusted, experienced medical team.