MR Linac Therapy
Introduction
In cancer care, the primary goal is to destroy tumor tissue while sparing healthy organs as much as possible. MR Linac therapy brings together external-beam radiotherapy with real-time magnetic resonance imaging (MRI), allowing clinicians to visualize both the tumor and nearby organs continuously during treatment and direct radiation with high precision.
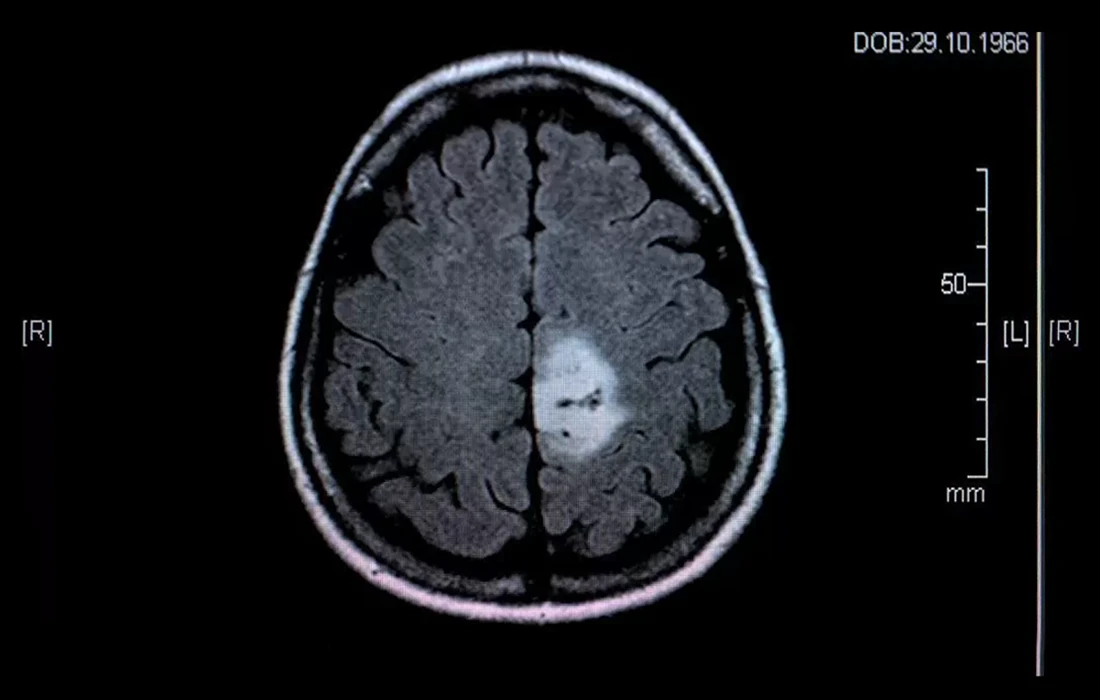
Unlike conventional radiotherapy—where the plan is created beforehand and delivered without continuous soft-tissue visualization—an MR-guided system can monitor the tumor live and adapt the beam as needed. This is particularly valuable for lesions in or near critical structures such as the brain, spinal cord, prostate, pancreas, and liver.
How MR Linac Therapy Works
An MR Linac integrates two technologies in a single device: A linear accelerator that generates therapeutic X-rays, and an MRI scanner that provides high-contrast, soft-tissue imaging. During each session, the system tracks the tumor’s live position (including respiration-related motion) and can adjust beam direction or shape accordingly. For a clear, patient-friendly overview, see RadiologyInfo’s explainer on MRI-guided Linac here.
Safety of MR Imaging
MRI uses magnetic fields and radio waves and therefore does not involve ionizing radiation. This means the continuous “live” visualization during MR Linac therapy does not add extra radiation exposure in the way a CT-based workflow would. Frequent MRI during a session is considered safe for patients.
When Is It Used?
MR Linac is especially helpful for tumors close to critical organs or in sites that move with breathing:
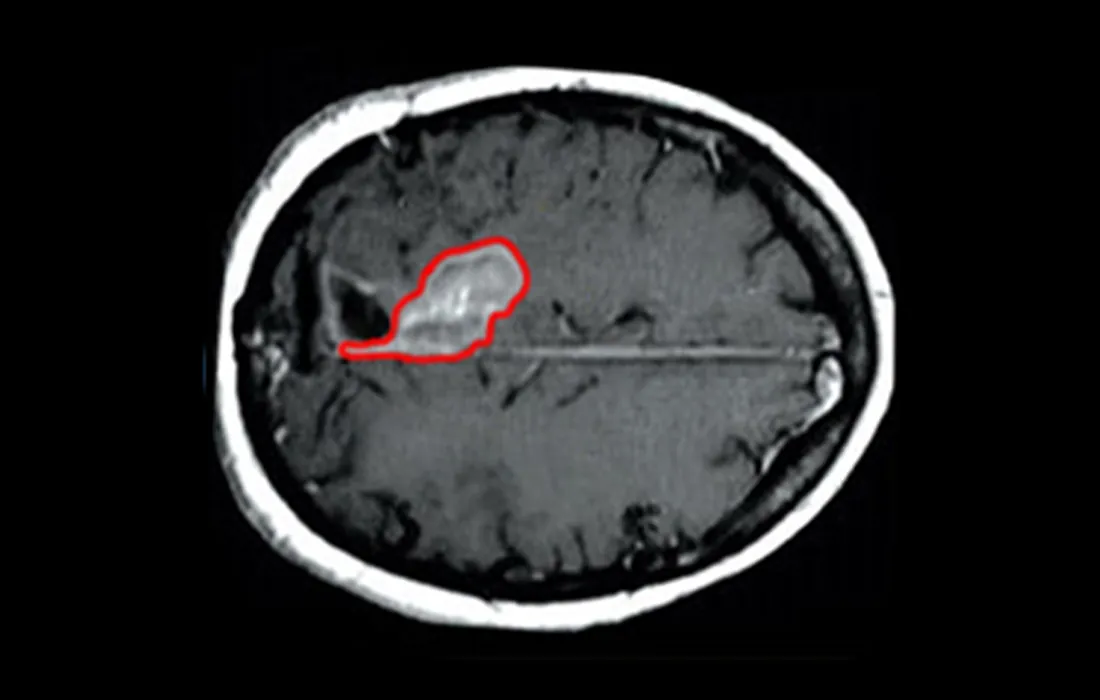
- Brain tumors: When surgery is risky or residual disease remains after surgery.
- Spinal cord tumors: For lesions where surgical morbidity would be high.
- Prostate cancer: High soft-tissue contrast improves targeting next to bladder and rectum
(see MD Anderson’s MR-Linac overview here). - Pancreas and liver tumors: Real-time tracking helps compensate for respiratory motion.
- Inoperable cases: A non-surgical, organ-sparing alternative when surgery is not feasible.
How Treatment Is Delivered
Planning: High-quality MRI is acquired to delineate the tumor and nearby organs; a personalized plan is created.
Each session: The patient lies on the treatment couch while MRI provides continuous visualization of the target.
Sessions are non-invasive and typically last 30–90 minutes. Patients do not feel the radiation; remaining still is important.
Total course: Depending on diagnosis and technique, it may range from a few sessions to 1–6 weeks (often 5 days/week).
Selected cases may receive a single, high-dose ablative session.
After the Session
Because this is not surgery, most patients get up immediately after treatment and go home the same day. Many resume light daily activities right away. Follow-up visits and imaging assess tumor response (shrinkage, stability, or complete response).
Advantages of MR Linac Therapy
- Live imaging: Continuous, high-contrast MRI of the tumor and organs during delivery.
- Precision: Real-time adaptation improves targeting and spares healthy tissue.
- Potentially fewer side effects: Reduced unnecessary dose to normal tissues.
- Surgical alternative in select cases: Particularly when surgery is high-risk or not possible.
- Patient comfort: Non-invasive, outpatient sessions; same-day return home.
For a clinical, peer-reviewed overview of MR-guided adaptive radiotherapy, see this open-access review on PubMed Central here.
Possible Side Effects of MR Linac Therapy
Side effects tend to be milder than with conventional workflows but depend on the treated area. Common issues include temporary fatigue, mild skin reactions over the entry site, and organ-specific symptoms such as headache/nausea (brain), gastrointestinal upset (abdomen), or urinary frequency/irritation (prostate).
Most effects are transient and manageable.
Expected Outcomes of MR Linac Therapy
Goals include tumor shrinkage or durable local control. Outcomes vary by tumor type, size, location, and overall patient health. In some cases, a complete response is achievable; in others, disease control and preserved quality of life are realistic targets. MR Linac may also complement surgery by treating residual disease post-operatively.
Who May Not Be Eligible?
- Patients with non-MRI-compatible implants (e.g., some pacemakers, certain neurostimulators) or ferromagnetic hardware.
- Extensive metastatic disease where focal control has limited impact on overall outcome.
- Individuals unable to lie still long enough to complete a session safely.
- Pregnancy, due to broader radiotherapy considerations.
Conclusion
MR Linac therapy is a modern, precise, and patient-friendly option for select brain, spine, prostate, pancreas, and liver tumors.
By combining radiotherapy with real-time MRI, it enhances accuracy and can reduce side effects, while allowing most patients to go home the same day.
In Türkiye, this technique is currently available in a limited number of experienced centers. For personalized guidance, eligibility assessment, and detailed information about MR Linac therapy, please contact us directly.